MSc. David Oliva Uribe
Uribe graduated in Electronic and Communication Engineering and obtained a Master in Sciences with Specialization in Manufacturing Systems, both at Tecnológico de Monterrey in Mexico City. Before starting at the Vrije Universiteit Brussel (VUB), Uribe was a team leader at the Institute of Dynamics and Vibrations Research at the Leibniz University of Hannover. Since January 2011, he is part of the Department ELEC at the VUB, where he is working toward a joint PhD degree. The intelligent surgical tool is his project.
How does the device work?
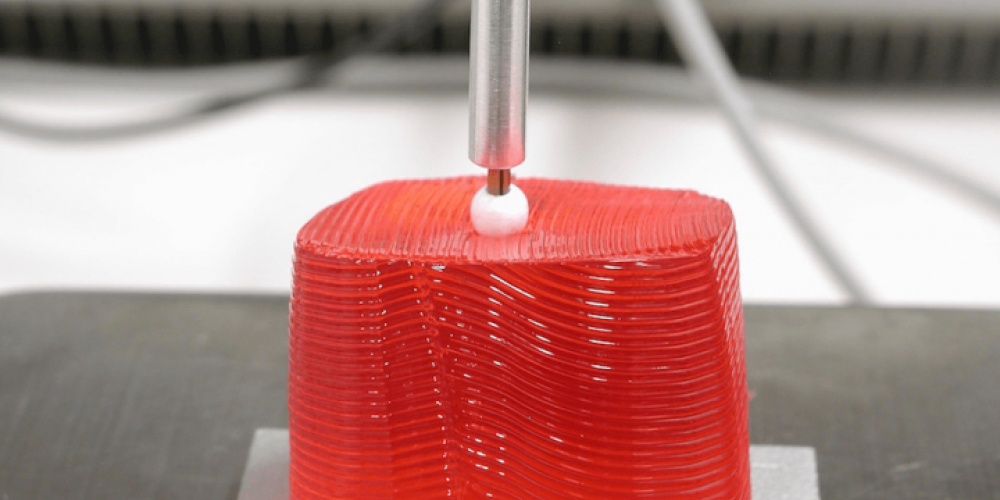
“The device is based on self-sensing actuators using piezoelectric transducers. The actuator generates vibration on the tip of the instrument. When the device comes across brain tissue, the vibration is induced into the tissue and the device realizes the estimation of the mechanical properties of the evaluated area. This measurement is then compared to a reference value previously taken on a well-known healthy area. Like this, the device can determine whether the tissue is healthy or tumorous. The time to evaluate a testing point currently takes around 400 milliseconds, which allows a real-time evaluation.”
Has the tool been tested on living subjects?
“The device has been successfully tested on artificial brain tissue and animal brains. The results showed the capability of the device to perform tissue differentiation with high accuracy. At the moment we are working to arrange testing on living subjects with our medical partners in Germany. We still have a lot of work to do in preparation of this though. Adaptations on the device and in the operating theater will have to be done to assure the safety of the patients. The testing on living subjects still requires a couple of years to be finished. Although this sounds like a long time, it is nothing unusual for medical development.”
What does this mean for the medical world?
“Currently there are two competing technologies to improve brain tumor removal. On the one hand, the development of intra-operative imaging devices, like MRI or CT-scan. The main idea here is to place these machines inside the operating theater to take images of the patient and update the information of the localization of the tumor at different stages of the surgery. This adds additional complexity, increase of time, extra specialized personnel to operate the imaging machines and of course, higher costs to the hospitals.
On the other hand there is the development of intelligent surgical tools, like the one we are developing. This will allow the surgeon to improve the outcome of the standard surgical procedure. The surgeon will use the same tools he/she was trained to use, but with the confidence of having a measurement in real time of the condition of the brain tissue. This technology leads to a safe tumor removal, which in turn leads to an increase of life expectancy after surgery. In addition, the costs of developing this tool are significantly lower.”